
By Dr. Helena G. Shannon, M.D., MOGA
OOctober. The month breast cancer gets to be center stage. PINK, PINK everywhere…NFL players in pink on the field, pink ribbons on signs around the country, pink mobile mammography vehicles in business parking lots. Wonder why all this fuss about breast cancer and making people aware? Could it be that awareness SAVES LIVES?
I am Helena Shannon, a board certified OBGYN physician, and have been in practice at MOGA for 11 years, which officially makes me unable to say “I am one of the young doctors at MOGA” anymore. Also important is that I am a breast cancer survivor. I was diagnosed at 37 years old. I had a 4 month old son, Jack Thomas, at the time of my diagnosis. I went through 8 cycles of “bad chemo,” 12 months of immunotherapy, double mastectomy, 25 cycles of radiation and breast reconstruction. That was 4 years ago and I am still in remission. The biggest silver lining about this diagnosis was that I lost all of my hair, sans about 5 eyelashes, in April so I had to shave nothing from April to October (i.e. “swimsuit season”). I guess if you have to get cancer, do it in the spring. Ha! Well on to it…
Breast cancer is the most common non-skin cancer in females. It is the leading cause of cancer death in females worldwide and the 2nd leading cause of cancer death in females in the US. A woman at average risk, the majority of women, has a 15% chance of developing breast cancer in her lifetime. That means it personally effects about 1 in 7 women. We know that screening does not prevent cancer but it certainly decreases deaths due to breast cancer, i.e. it SAVES LIVES, by detecting it at earlier stages.
A screening mammogram is done on average risk patients with no signs or symptoms of breast cancer. A diagnostic mammogram is done on patients with signs or symptoms (mass, nipple discharge, thickened skin or nipples, pain, changes in breast size or shape), at higher than average risk and as follow up for abnormal screenings. Breast ultrasound and MRI may be used for follow-up of abnormal findings on or to supplement screening/diagnostic mammogram but shouldn’t be used in to replace mammogram. Don’t get me wrong, mammograms are in no way perfect in detecting every case of breast cancer but they are the best option we have. Also 1 in 10 women will have an abnormal screening mammogram and get the dreaded “we need more imaging” phone call causing immeasurable anxiety. The good news…most patients with abnormal screenings do NOT have cancer. “Screening” can also apply to breast self examination (BSE) and clinical breast examination (CBE) done by your physician on a yearly basis.
SBE does not increase the rate of breast cancer diagnosis or decrease the rate of breast cancer death but does increase the number of biopsies for benign breast lesions. Does this means that you should ignore your breasts? Absolutely not! Any breast concern should be promptly addressed with your clinician. Do not be reluctant/hesitant to come because you don’t want to feel “stupid” or “waste my time” for something that is likely benign. I assure you, you will NEVER waste my time or feel “stupid” coming to
see me.
CBE is not as good as mammogram in detecting breast cancer but may be used in addition, not as a replacement, to mammography. CBE may detect 5% of cancers not seen on mammogram.
The bottom line, breast cancer is common- a 15% lifetime risk- and screening is very accessible, mammograms require no clinician’s order, takes 10-20 minutes and SAVES LIVES. We offer in-office screening mammograms at all of the MOGA locations. Don’t be afraid of getting cancer; focus on staying alive.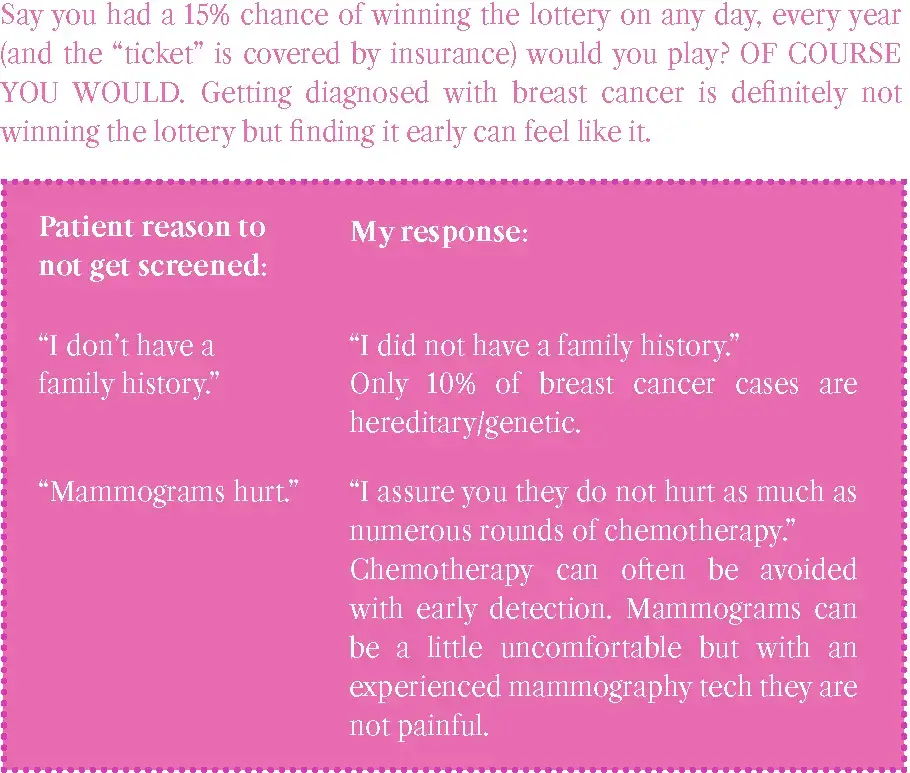
Share Let's Catch Some Cancer

